Choline is a crucial nutrient for gut, skin, neurological, and cellular health. Yet, according to the 2003-2004 National Health and Nutritional Examination Survey (NHANES), only 10 percent of Americans consistently meet the adequate intake for choline (1).
Choline also plays essential roles during growth and development, and the body’s need for choline increases during pregnancy. The amniotic fluid surrounding the baby in the womb is highly enriched with 14 times the level of choline found in the mother’s blood (2). Sadly, an estimate from 2014 indicates that 90 to 95 percent of women fail to meet recommended choline intakes during pregnancy (3).
Additionally, new research has identified human gut bacteria that can compete with the host for choline. This means that those with gut dysbiosis, and particularly those with small intestinal bacterial overgrowth (SIBO), could be at risk for choline deficiency, even if they are consuming choline-rich foods or taking choline supplements.
In this article, I’ll cover all of the relevant research surrounding choline for general health and pregnancy, including the role of our gut microbes, and discuss how we can use this information to optimize choline status.
The importance of choline
Choline carries out many important functions in the body. It is an essential component of phospholipids, which make up the structure of cell membranes. Choline is also a precursor to the neurotransmitter acetylcholine, which plays roles in memory, circadian rhythms, and muscle control, and sphingomyelin, which is found in the fatty sheath around nerve fibers and improves the conduction of electrical impulses. The transport of fat and cholesterol from the liver also requires choline, and deficiency can lead to non-alcoholic fatty liver disease (NAFLD) (4).
9 out of 10 Americans don’t get enough choline, and deficiency may be especially harmful during pregnancy. Certain gut microbes could prevent proper choline absorption. Learn how to optimize your choline status to support overall health.
Choline is also an important source of methyl groups. The addition of methyl groups to the DNA structure can turn genes on or off without any changes to underlying DNA sequence, a process known as epigenetics. Epigenetics plays an important role in health throughout life but is particularly important during growth and development, as fetal stem cells divide and differentiate into organs with all kinds of complex cellular functions. Changes in DNA methylation have been associated with cancer, aging, cognitive disabilities, atherosclerosis, and autoimmunity (5).
In utero, choline status also has implications for the structural development of the hippocampus, the primary brain region responsible for learning and memory (6). Poor maternal choline status may also increase the risk of neural tube defects and impair development of the heart (7).
So how much choline do we need?
Unfortunately, there is still a lack of consensus on exactly how much choline we need. The Institute of Medicine, which establishes the RDAs for nutrients based on peer-reviewed studies, has been unable to come up with a definitive value for choline needs and has had to resort to establishing an “Adequate Intake” value for choline (8). This is sort of a “best guess” as to how much choline might be sufficient for most people.
Below are the adequate intake values for choline (9):
Infants (0–6 months old): 125 mg per day
Infants (6–12 months old): 150 mg per day
Children (1–2 years old): 200 mg per day
Children (4–8 years old): 250 mg per day
Children (9–13 years old): 375 mg per day
Adult men: 550 mg per day
Adult women: 425 mg per day
Pregnant women: 450 mg per day
Lactating women: 550 mg per day
Chris Masterjohn has previously explained why trying to estimate how much choline we need is almost impossible. He has also extensively discussed the factors that influence dietary choline requirements, including genetic variations, intake of other B vitamins (particularly other methyl donors), and overall energy intake. Thus, I won’t be discussing any of these factors here. Since the microbiome is my area of expertise and the newest identified factor affecting choline status, the rest of this article will focus on gut bacterial influences on choline requirements.
Microbes compete for host choline
A recent study from the lab of leading microbiome researcher Dr. Federico Rey suggests that our gut microbes may influence choline status (10). I find this fascinating, but if you get bogged down in the details, you can skip ahead to the end of this section, where I’ll discuss the implications of this research!
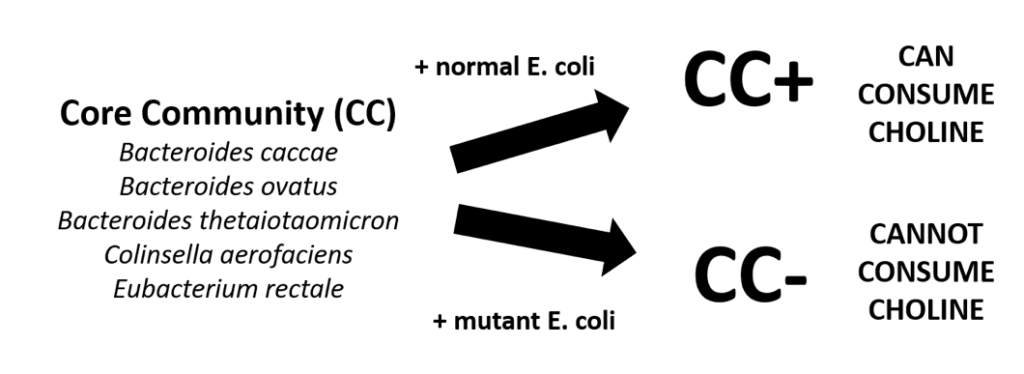
This study used what are known as gnotobiotic (know-toe-by-ah-tic) mice. These are mice colonized with a known community of microbes. In this case, the researchers chose a core community (CC) of five microbes that are abundant in the normal human gut. To half of the mice (CC+), they also added a strain of E. coli that is known to metabolize choline. To the other group (CC-), they added the same strain of E. coli, but mutated the enzyme responsible for choline metabolism. Thus, the only difference between the groups was that one could utilize choline, while the other could not.
The researchers then took blood samples and found that CC+ mice had very low levels of serum choline compared to CC- mice. This suggested that the E. coli microbe was competing with the host for choline.
Moreover, they found that CC+ mice had lower levels of DNA methylation that mimicked those seen in choline deficiency. To explore the implications of these altered methylation profiles, Dr. Rey and colleagues repeated the experiments in mouse models of metabolic syndrome and pregnancy and early life.
- In the metabolic disease model, CC+ mice had increased circulating leptin, increased blood triglycerides, and fatty livers compared to CC- mice.
- In pregnancy, mother CC+ mice had increased obsessive grooming behavior, and their offspring showed increased marble-burying behavior, indicative of increased anxiety.
So, what are the major takeaways? First, gut bacteria may impact choline bioavailability in ways that mimic outright choline deficiency. Therefore, we can’t just be concerned with the adequate intake for choline, as individual needs for dietary choline are dependent on the gut microbiome. This study also suggests that excessive bacterial metabolism of choline could be especially harmful in pregnant women and those with metabolic syndrome.
Could SIBO be causing choline deficiency?
Additionally, what most people didn’t catch in the methods of this study is that the choline-hungry E. coli strain used in the study is a robust colonizer of the small intestine.
To help convey the importance of this, I should review some basic gut anatomy. Food passes through the stomach to the small intestine, and then through the large intestine. It’s no mistake that the small intestine, the primary site of nutrient absorption, is upstream from the large intestine, which is home to the bulk of the gut microbiota. In a healthy individual, this arrangement ensures that our epithelial cells have “dibs” on any incoming nutrients, and our microbes get the “leftovers.”
In small intestinal bacterial overgrowth (SIBO), however, the pecking order changes. Microbes from the colon move up the gastrointestinal tract to colonize the small intestine, or small intestinal microbes flourish and become overgrown. These microbes now directly compete with the host for any incoming nutrients—and in many cases, they win out. SIBO may particularly affect host status for nutrients absorbed in the lower small intestine, such as iron, vitamin B12, and—based on this research—choline.
In other words, those with SIBO may be at particularly increased risk for choline deficiency. (This remains to be confirmed in humans, but the microbial strain used in this mouse study was isolated from the human gut.)
Could high circulating TMAO be linked to SIBO?
What is most intriguing is that choline bacterial metabolism also leads to high serum levels of TMAO (trimethylamine N-oxide). TMAO has received a great deal of attention for its associations with cardiovascular disease (11). Bacteria convert choline to TMA, which is then oxidized in the liver to TMAO. Chris has talked about TMAO before on both his blog and his podcast, suggesting that high serum TMAO levels are more about which gut microbes you have and less about how much choline and carnitine you consume. The study I outlined above provides support for this hypothesis: CC+ mice had much higher levels of TMAO, while CC- mice had virtually undetectable TMAO.
Additionally, preliminary data from the Rey lab has shown that in humans, low serum choline tends to be associated with high TMAO, and vice versa. If TMAO was primarily being produced from “leftover” choline in the colon, we likely would not see this relationship. This suggests that those with high TMAO are very likely harboring some form of SIBO—further explaining the connection between SIBO and cardiovascular disease. Indeed, a 2017 study confirmed that TMA is only absorbed in the small intestine. Moreover, an acute dose of rifaximin, the non-absorbable antibiotic most commonly used to treat SIBO, can reduce serum levels of TMAO (12)!
Could betaine help overcome choline deficiency?
In thinking about solutions to choline deficiency, it’s important to note that one of choline’s most important roles in physiology, that of a methyl donor, first requires the conversion of choline to betaine. In other words, it’s betaine that acts as the direct methyl donor. Betaine cannot completely fulfill choline requirements, since choline has several functions besides methylation, but it can help prevent some of the epigenetic consequences of choline deficiency.
While betaine can also be consumed by microbes (and lead to TMAO production), betaine is primarily absorbed high in the proximal (upper) small intestine, whereas choline is absorbed lower, primarily in the distal (lower) small intestine (13). Since SIBO is most common in the distal small intestine, this means that, theoretically, betaine may have a better chance to be absorbed than choline. Of course, this is all speculation, and I look forward to seeing more studies in this area.
Additionally, I’d muse that consuming both betaine and choline may increase the chances that at least one is absorbed, since different bacterial species compete for each of these two nutrients. Many people with SIBO supplement with betaine HCl to help correct low stomach acid—but betaine HCl may also help compensate for bacterial choline metabolism in the small intestine and prevent symptoms of choline deficiency.
How to optimize choline status
Putting all of this information together, there are several steps we can take to help optimize choline status (even if we don’t know exactly how much we need):
- Treat SIBO and gut dysbiosis: As always, we want to treat the underlying cause of disease. In this case, if SIBO is contributing to choline deficiency, addressing SIBO may improve choline status. This involves taking antimicrobials, improving gut motility, and restoring adequate stomach acid levels. Klebsiella and Escherichia appear to be particularly thrifty choline consumers.
- Consume plenty of choline-rich foods: the top whole-food sources of choline are listed below. Human breast milk is also rich in choline.
- Beef liver (3 oz.): 356 milligrams
- Eggs (1 whole): 147 milligrams
- Beef round steak (3 oz.): 117 milligrams
- Supplement with (phosphatidyl)choline: For those who cannot get sufficient choline from dietary sources, I recommend supplementation. It’s important to note that most prenatal supplements and multivitamins do not contain choline, and those that do often contain the choline chloride form.
I recently had the opportunity to ask Dr. Rey about his thoughts on various choline supplements. He suggested that while all forms of choline are used by microbes, phosphatidylcholine seems to take more work for the microbes to utilize and may have a better chance of being absorbed than compounds like choline chloride. This is also the form found naturally in most foods. I like Seeking Health Optimal PC.
While it’s possible that consuming extra choline may fuel the overgrowth of choline consumers, the consequences of inadequate choline are far too great to even consider restricting choline intake.
- Consume betaine-rich foods: as I discussed above, consuming adequate betaine may reduce the need for choline. The top three whole-food sources of betaine are:
- Beets (1 cup, raw): 175 mg
- Spinach (1 cup, cooked): 160 mg
- Sweet potato (1 medium): 39 mg
- Supplement with betaine: For those with SIBO and inadequate stomach acid secretion, betaine HCl is an excellent choice. I recommend one to five capsules, as tolerated, taken with meals.
I’d love to hear from you. What do you think of the research? Do you get enough choline and betaine? Share your thoughts in the comments!
 About Lucy: Lucy is an MD-PhD student in Nutritional Sciences at the University of Illinois and a staff research associate for Kresser Institute. Her laboratory research focuses on the effects of diet and exercise on the gut microbiome and how this impacts gut and skin health. She was recently recognized as an emerging leader in Nutritional Sciences by the American Society for Nutrition and has contributed to several peer-reviewed publications.
About Lucy: Lucy is an MD-PhD student in Nutritional Sciences at the University of Illinois and a staff research associate for Kresser Institute. Her laboratory research focuses on the effects of diet and exercise on the gut microbiome and how this impacts gut and skin health. She was recently recognized as an emerging leader in Nutritional Sciences by the American Society for Nutrition and has contributed to several peer-reviewed publications.
Lucy’s mission is to provide evidence for an individualized, integrative approach to health through innovative research and outstanding clinical practice. She recognizes that each individual is unique, and she currently helps clients with gut, skin, and autoimmune conditions. You can learn more about her at NGmedicine.com or join her weekly newsletter here!
The post Choline, SIBO, and Pregnancy: What’s the Deal? appeared first on Chris Kresser.
from Chris Kresser https://chriskresser.com/choline-sibo-and-pregnancy-whats-the-deal/
via Holistic Clients

No comments:
Post a Comment